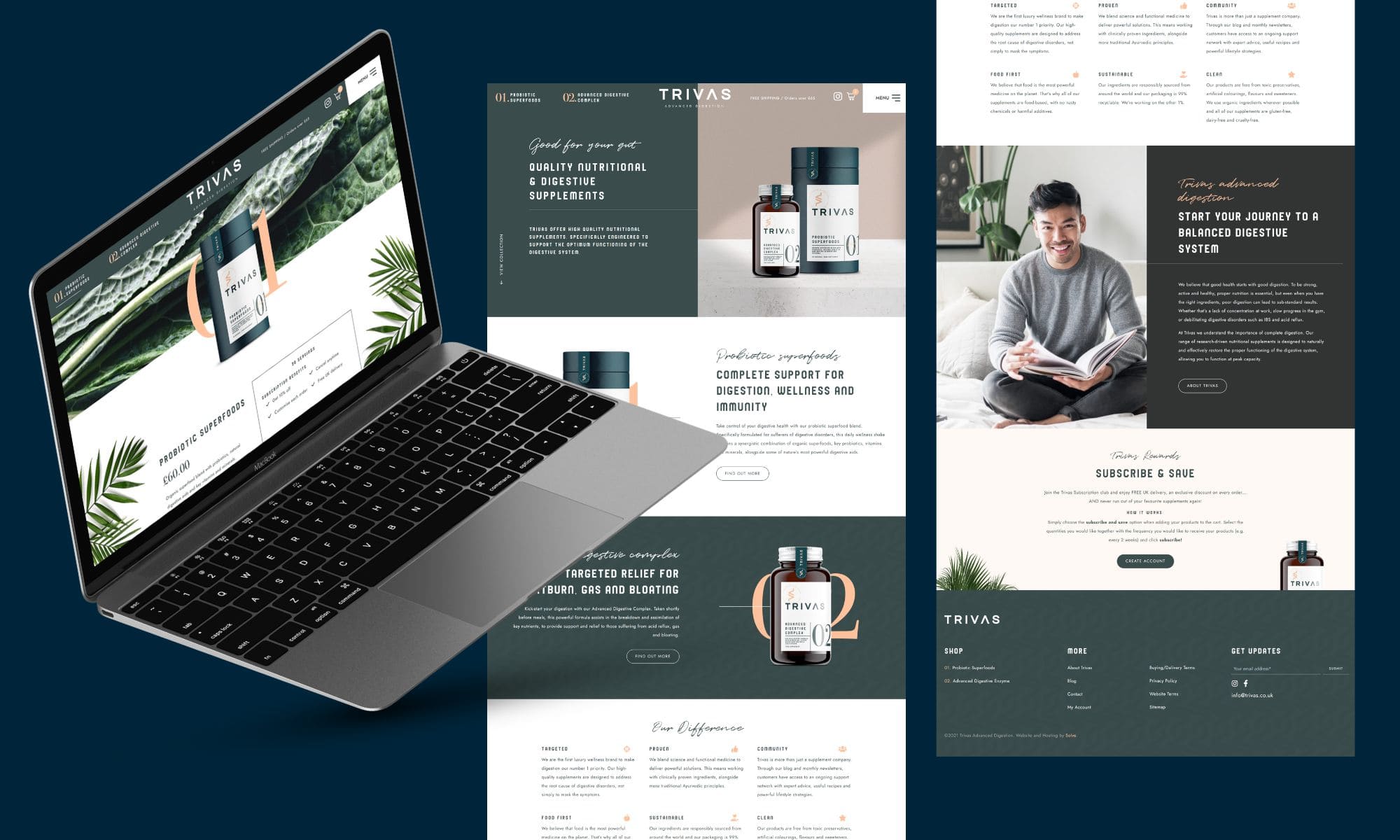
Trivas offer high-quality nutritional supplements, specifically engineered to support the optimum functioning of the digestive system. They aim to create a community of like-minded individuals living active, successful lives without the burden of digestive discomfort.
With Trivas’ website, we were determined to create something as unique as the offering itself – creating a bespoke design that worked seamlessly with their branding. We also made sure to build in recommended SEO fundamentals and carried out detailed keyphrase research from the ground up, allowing for the site to be indexed correctly by Google and maximise its potential.
- Website design and development
- SEO Foundation (Level 1)
- Optimised hosting + support
- SSL + support
- E-Commerce WordPress maintenance
- Pro CDN + support